Introduction
Varicose veins are extremely common in our population, accounting for 30 to 50 percent of women and 20 to 30 percent of men.
This disease will be more and more frequent due to the aging of the population and the increasing problems of lifestyle.
For nearly a hundred years, the explanation and the methods of treatment of varicose veins have evolved little. The aggressiveness of surgical treatment (removal of the saphenous vein by stripping), the repetitive nature of sclerosis treatments, the discomfort of wearing compression stockings, and the frequency of recurrences very often discouraged patients.
At the dawn of the 21st century, new, less aggressive techniques appeared that allowed the saphenous vein to be removed without actual surgery (laser, radiofrequency, foam echosclerotherapy). More recently, a new conception of the development of varicose disease has called into question the the principle of systematic removal or destruction of the saphenous vein with, in many cases, the possibility of preserving the saphenous vein, which can recover satisfactory function (ASVAL method).
Thus, real revolutions in the explanation and treatment of varicose veins have been taking place over the last few years. Their objectives are to be preventive, less aggressive and more precise. This allows patients to be treated better, earlier and with a better follow-up.
Physiology, anatomy, origin and consequence of varicose veins
 Physiology
Physiology
Veins are used to bring blood from the tissues back to the heart, unlike arteries which carry it from the heart to the organ.
Thus, at the level of the legs, in a standing or sitting position, the veins must bring the blood up to the heart, against gravity.
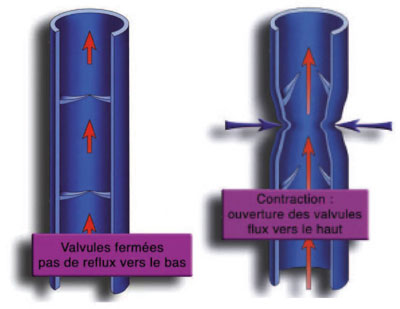
To allow the blood to flow upwards, the veins are equipped with anti-reflux valves, called “valves”, which allow the blood to flow upwards and prevent it from falling back towards the feet.
During leg movements, especially when walking, muscle contractions and joint movements crush the veins, which causes blood to flow upwards through the valves.
Anatomy
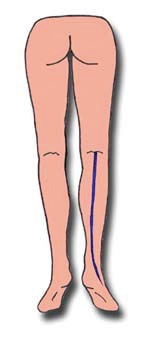
There are two main superficial veins in each lower limb :
Les veines saphènes sont les collecteurs du sang veineux venus des branches ou collatérales. Varicose veins are developed on these branches where reflux develops (reversal of flow diagnosed by Doppler examination). The saphenous veins are secondarily affected by reflux when the varicose disease is worsening.
Origin of varicose veins
Most often this disease is linked to a weakness of the venous wall, probably transmitted by heredity. This weakness will progressively worsen throughout life, encouraged by risk factors: jobs involving prolonged standing and walking, weight gain, pregnancy, heat, risky activities, etc…
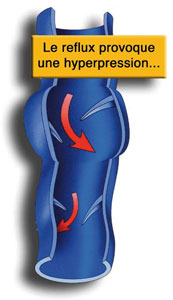
The vein wall will eventually dilate, the valves will spread, letting the blood leak downwards (reflux). This reflux will lead to an increase in pressure in the vein (hyperpressure). The dilation becomes permanent: it is a varicose vein.
A vicious circle will be created :

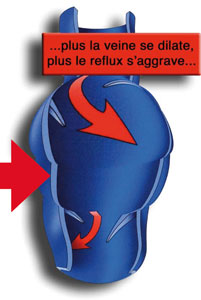
This phenomenon of reflux will extend from proximal to proximal veins, and contaminate an increasingly extensive superficial venous network on the branch network and then from the branches to the saphenous vein.
Consequence of varicose veins
Aesthetic consequences
Spider veins or telangiectasias are skin veins, as thin as hair, in the shape of stars or spider legs, blue, purple or red in color, generally very apparent. They precede varicose veins, which are larger, dilated and very unsightly veins.
Consequences on comfort living
Varicose veins can be responsible for pain, unpleasant heaviness, tingling, itching, or restless syndrome. These signs predominate especially in the evening, after a day of walking, when it is hot, before menstruation or during pregnancy. Night cramps could also be linked to varicose veins.
Health consequences
Edema appears more or less quickly, then skin disorders progressively: brown spots appear, the skin becomes hard and fragile, with a risk of varicose ulcer.
Acute complications can appear, even when varicose veins only represent an aesthetic embarrassment: superficial phlebitis, or more rarely, hemorrhagic rupture.
Patho-physiology of varicose veins
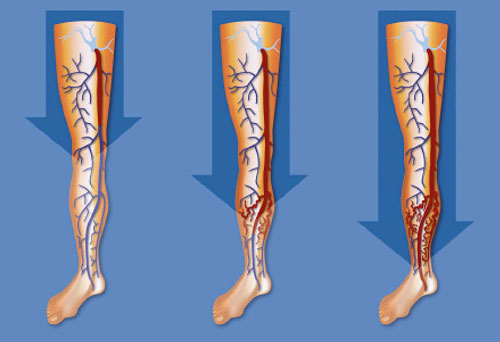 The old traditional theory of varicose disease was described in 1890 (1): elle explique l’apparition des varices à partir d’une dégradation de la veine saphène, depuis le pli de l’aine ou le creux du genou, de façon descendante vers la cheville, avec un reflux qui va progressivement faire apparaître les varices sur les branches collatérales.
The old traditional theory of varicose disease was described in 1890 (1): elle explique l’apparition des varices à partir d’une dégradation de la veine saphène, depuis le pli de l’aine ou le creux du genou, de façon descendante vers la cheville, avec un reflux qui va progressivement faire apparaître les varices sur les branches collatérales.
This description therefore makes the saphenous vein “responsible” for the development of varicose veins on its branches.
It was thus logical that the traditional treatment of varicose veins consisted in removing the saphenous vein, at the origin of the development of varicose veins according to the usual theory.
Treatements to remove the Saphenous vein
The stripping
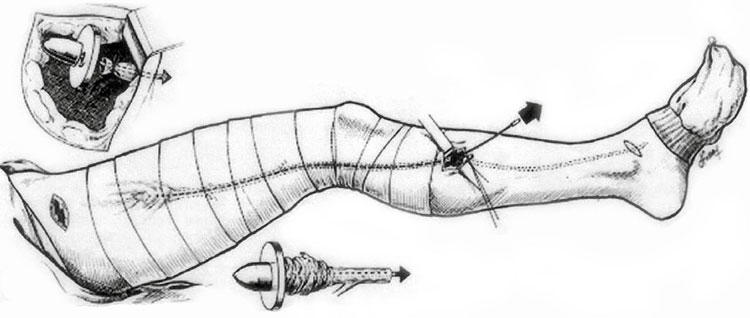 It is a technique described in 1906 (2), which consists in removing the saphenous vein from its termination at the fold of the groin for the great saphenous vein, or the hollow of the knee for the small saphenous vein to the calf, at a variable level.
It is a technique described in 1906 (2), which consists in removing the saphenous vein from its termination at the fold of the groin for the great saphenous vein, or the hollow of the knee for the small saphenous vein to the calf, at a variable level.
This technique is still widely practiced in France, in nearly 90% of cases in a study conducted in 2003 (3) and still 50% of cases according to current data from the CPAM.
It is performed under general or loco-regional anesthesia (equivalent to epidural), with a full day or overnight hospitalization (4).
Stripping is often completed by the removal of varicose veins (phlebectomy) on the branches, through additional incisions during the same operation.
The time off work following the operation is generally 15 days to 1 month.
Endovenous treatments
Endovenous laser and radiofrequency were described in the early 2000s (5,6). These techniques consist in removing the saphenous vein by heat thanks to a probe that is introduced through the skin inside the saphenous vein, without having to make an incision at the level of the fold of the groin or the hollow of the knee.
Endovenous techniques represent an improvement in that they are much less aggressive and are performed under local anesthesia without hospitalization.
Endovenous treatments have developed a lot in North America and in many European countries, while they are still relatively undeveloped in France (only in half the cases).
It should be specified that these endovenous techniques only allow the removal of the saphenous vein and not the removal of the varicose veins which are developed on the branches. As for stripping (see above), the treatment of varicose veins will thus require either a surgical procedure (phlebectomy) through small incisions.
Foam echosclerotherapy
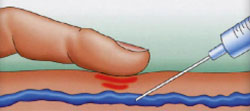 This technique, described in 1993 (7), consists of injecting a sclerosing product in the form of a foam into the saphenous vein, under ultrasound control, leading to its chemical destruction in the more or less long term in a significant proportion of cases (between 60 and 90%), depending on the number of injections performed.
This technique, described in 1993 (7), consists of injecting a sclerosing product in the form of a foam into the saphenous vein, under ultrasound control, leading to its chemical destruction in the more or less long term in a significant proportion of cases (between 60 and 90%), depending on the number of injections performed.
It requires neither anesthesia nor hospitalization.
It can also be used to treat varicose veins on the branches, but requires several sessions to be effective.
Endovenous treatments and foam echosclerotherapy represented a first revolution in the treatment of varicose veins because of their less aggressive nature, the absence of major anesthesia, hospitalization, postoperative disability, and no or very little time off work.
However, none of the treatments aiming at suppressing the saphenous vein makes it possible to “cure” the disease of varicose veins, insofar as the reappearance of varicose veins after a few years is extremely frequent, from 30% at 5 years to more than 80% more than 10 years after an intervention.
New conception of varicose disease and new treatment
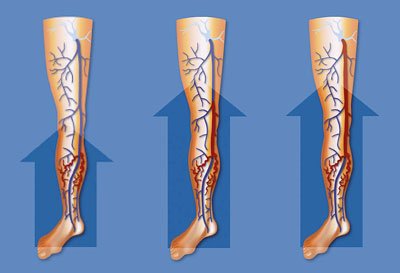 A radically different conception of the direction of evolution of varicose disease has been reported more recently by several authors(8,9,10): it evokes the development of varicose veins from the branches, in an ascending manner, towards the saphenous vein.
A radically different conception of the direction of evolution of varicose disease has been reported more recently by several authors(8,9,10): it evokes the development of varicose veins from the branches, in an ascending manner, towards the saphenous vein.
The saphenous vein would only be affected secondarily, “contaminated by the varicose veins developed on the branches. The saphenous vein would thus be the “victim” of varicose veins, affected at a later stage, and not the “responsible” one at the origin of varicose veins.
Two elements led to the development of this revolutionary theory:
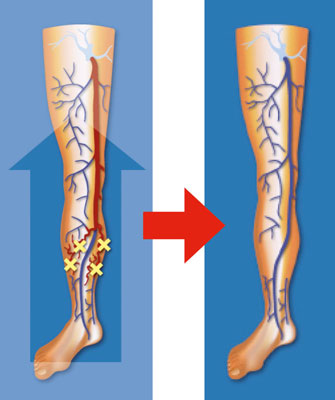 A new treatment principle based on this new theory was therefore described in 2003 (14), the ASVAL method (Selective Ablation of Varicose Veins under Local Anesthesia). This method consists of removing only the diseased branches, while preserving the saphenous vein. The objective of this method is to prevent the saphenous vein from being affected if the disease is still limited to the branches, or to “recover” the saphenous vein if it is already affected by reversible reflux.
A new treatment principle based on this new theory was therefore described in 2003 (14), the ASVAL method (Selective Ablation of Varicose Veins under Local Anesthesia). This method consists of removing only the diseased branches, while preserving the saphenous vein. The objective of this method is to prevent the saphenous vein from being affected if the disease is still limited to the branches, or to “recover” the saphenous vein if it is already affected by reversible reflux.
Varicose veins are removed through tiny incisions (microphlebectomies by microincisions of 1 mm) that do not require any postoperative care (no dressing, no stitch removal).
This method does not require significant anesthesia (only local anesthesia) and does not require hospitalization, as the patient returns home one hour after the procedure, without any post-operative disability. It is even strongly recommended to walk 3 to 5 km as soon as you leave the clinic and then twice a day for the following days.
The studies (15,16) on the ASVAL method have shown its interest in the simplicity of the postoperative period, with almost no pain, bruising, or time off work.
Recently, a study presented in the United States by our team (17) showed the quality of the results 4 years after the operation: improvement of the discomfort linked to varicose veins (pain, heaviness, aesthetic discomfort) in more than 80% of cases, with a total or partial recovery of the saphenous vein in more than 90% of cases.
The ASVAL method is a real revolution (it is the subject of numerous international communications) because it is centered on the treatment of varicose veins developed on the collateral branches :
The ASVAL method, like the other techniques, does not claim to cure varicose vein disease because the risk of recurrence remains present due to the patient’s personal terrain. It therefore requires regular follow-up to avoid the return of major varicose veins.
Its major advantage is that it is effective (the varicose veins are removed), adapted to each patient (à la carte treatment according to the patient’s personal pattern), with a very gentle technique (local anesthesia, micro-incisions, no post-operative care).
The ASVAL method is used by our team on more than 80% of patients treated for varicose veins.
Conclusion
The treatment of varicose veins evolved very little throughout the 20th century. The change of millennium coincided with the appearance of new, less aggressive, minimally invasive endovenous techniques, followed by a veritable revolution, internationally recognized, in the explanation and management of varicose disease, with the ASVAL method developed by Dr. Pittaluga’s team: a surgical technique under local anesthesia that is gentle, aesthetic, and respectful of the venous circulation.
The aftermath of these less aggressive treatments has been transformed, with far fewer inconveniences than usual (anesthesia, pain, dressings, work stoppage, discomfort in walking and in daily activities, etc.), and excellent results in terms of discomfort and aesthetics.
Post-operative follow-up has taken on its full importance, both in terms of medical monitoring and maintenance treatments, and in terms of repeated information on lifestyle advice.
This should allow patients to be treated as soon as the first varicose veins appear, without waiting for the onset of significant pain or skin lesions.
The long-term result will be better, provided that the varicose veins have been treated early and in a targeted manner, and that the monitoring has been rigorous and effective.
Bibliography
- Trendelenburg F. Ueber die Unterbindung der Vena Saphena magna bei Unterschenkel Varicen. Beitr Klin Chir1890-1 ; 7 :195-210
- Mayo CH. Treatment of varicose vein. Surg Gyn Obst. Br J Surg 1906;2:385-388
- Perrin M, Guidicelli H, Rastel D. Résultats d’une enquête sur les techniques chirurgicales utilisées dans le traitement des varices. J Mal Vasc 2003; 28: 277-286.
- La chirurgie ambulatoire : potentiel de développement pour 17 gestes marqueurs. Bulletin d’information en économie de la santé. CREDES. N°50 – avril 2002 : 1-6
- Min RJ, Zimmet SE, Isaacs MN, Forrestal MD. Endovenous laser treatment of the incompetent greater saphenous vein. J Vasc Interv Radiol. 2001;12: 1167-71.
- Manfrini S, Gasbarro V, Danielsson G, Norgren L, Chandler JG, Lennox AF, Zarka ZA, Nicolaides AN. Endovenous management of saphenous vein reflux. Endovenous Reflux Management Study Group. J Vasc Surg. 2000 ;32 :330-42.
- Cabrera Garrido JR, Cabrera Garcia Olmedo JR, Garcia Olmedo D. Nuevo metodode esclerois en las varices trunculares. Pathologica Vasculares 1993 ; 1 : 55-72
- Labropoulos N, Leon L, Kwon S, Tassiopoulos A, Gonzalez-Fajardo JA, Kang SS, Mansour MA, Littooy FN. Study of the venous reflux progression. J Vasc Surg. 2005;41:291-5.
- Engelhorn CA, Enge lhorn AL, Cassou MF, Salles-Cunha SX. Patterns of saphenous reflux in women with primary varicose veins. J Vasc Surg. 2005;41:645-51.
- Pittaluga P, Chastanet S, Réa B, Barbe R, Guex JJ, Locret T. Corrélation entre l’âge, les signes et symptômes de l’insuffisance veineuse superficielle et les résultats de l’exploration écho-Doppler. Phlébologie 2006 ; 59 : 149-156
- Rutgers PH, Kitslaar PJ. Randomized trial of stripping versus high ligation combined with sclerotherapy in the treatment of the incompetent greater saphenous vein. Am J Surg. 1994; 168: 311-5
- Merchant RF, Pichot O. Long-term outcomes of endovenous radiofrequency obliteration of saphenous reflux as a treatment for superficial venous insufficiency. J Vasc Surg 2005;42:502-509
- Pittaluga P, Chastanet S. Classification of saphenous refluxes : implications for treatment. Phlébology 2008 ; 23 : 2-9
- Pittaluga P., Chastanet S. Réa B., Barbe R., Guex J.J. A.S.V.A.L. method: principles and preliminary results – In Becquemin JP, Alimi YS and Watelet J eds. Updates and controversies in Vascular Surgery. Torino : Minerva Medica, 2005, pp 182-189.
- Pittaluga P, Chastanet S, Marionneau N, Creton D, Lefebvre-Vilardebo M, Rea B, Sala F, Uhl JF. Traitement chirurgical des varices des membres inférieurs : approche moderne . Phlébologie 2004; 57: 301-307
- Pittaluga P, Chastanet S Rea B, Barbe R. Méthode ASVAL (Ablation Sélective des Varices sous Anesthésie Locale) : principes et résultats préliminaires. Phlébologie 2005 ; 2 : 175-181
- Chastanet S, Pittaluga P. Mid-term outcomes of incompetent saphenous vein preservation with phlebectomy (ASVAL method) as a treatment for superficial venous insufficiency. 21th Annual meeting of the American, College of Phlebology. Tucson (AZ) USA, le 10 novembre 2007




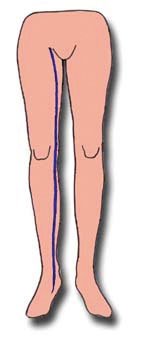 The long saphenous vein or great saphenous vein: between the medial part of the ankle and the groin crease, at the medial part of the calf and thigh.
The long saphenous vein or great saphenous vein: between the medial part of the ankle and the groin crease, at the medial part of the calf and thigh.