Vascular Surgeon
Expert in the treatment of varicose veins
I have varicose veins: where do they come from, how do they evolve, what symptoms do they cause and what can I do?
What are varicose veins ?

photo 1
The medical definition of varicose veins is the following:
- Varicose veins are dilated and elongated veins, permanently, which do not exert any more their role of drainage of venous blood.
- They appear in a more or less visible way under the skin, in the form of bluish cords, bumps or rosaries (photo 1).
- They are often unesthetic and sometimes painful.
- They are almost always located on the legs.
How and why do varicose veins appear?
The deformation by dilatation of the normal vein into a varicose vein is consecutive to a weakness of the vein wall, almost always of hereditary origin.

figure 1
When this dilation becomes permanent, a varicose vein appears on the legs (Figure 1).
This dilatation appears most often spontaneously, at a certain moment of life, often because of favorable situations, called “risk factors”, such as :
- aging
- sedentary lifestyle (lack of daily physical exercise)
- professional or daily life trampling
- weight gain
- pregnancy
- regular exposure to heat
- trauma to the leg
Are varicose veins more common in women and the in the elderly?
Large-scale studies show that varicose veins are not more frequent in women overall. On the other hand, they appear at a younger age in women, for hormonal reasons and due to pregnancy. In addition, women are more often treated than men because they suffer more (pain, aesthetic discomfort).
At the opposite, varicose veins are much more frequent with age; the older you get, the more likely you are to have varicose veins, especially if you have a hereditary condition. The average age at which one begins to be treated for varicose veins is in early fifties.
How do varicose veins evolve?
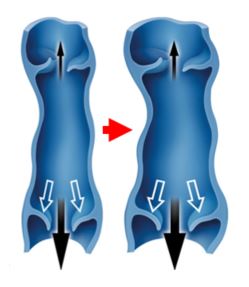
diagram 2
Varicose veins almost always worsen over time.
This worsening is explained by the dilation of the vein: this dilation leads to a separation of the valves which normally ensure the watertightness of the vein (see blog Functioning of the veins of the legs), letting the blood leak downwards, it is the “venous reflux”.
This “reflux” creates a local hyperpressure which accentuates the dilation, initiating a vicious circle which makes the vein swell more and more with time (diagram 2).
A varicose vein will also tend to progressively contaminate the neighboring veins, causing the varicose veins to spread throughout the venous network (Figure 3).
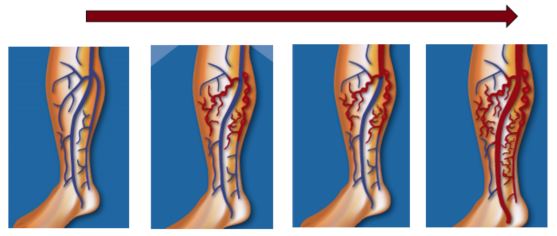
figure 3
How fast can varicose veins get worse?
The enlargement and extension of varicose veins are most often very progressive, over several years.
However the speed of evolution is variable from one individual to another, according to the fragility of the veins at the beginning (importance of the heredity) and according to the exposure of each one to the risk factors (see above).
Varicose veins can also suddenly worsen in an individual, whereas they were stable, due to a change in situation or personal context, making a risk factor appear or worsen.
Two very frequent examples:
- Pregnancy which will lead to the rapid aggravation of varicose veins which were not visible or which had remained limited until then.
- A change of professional situation leading to a significant trampling which will reduce the muscular activity and the venous drainage of the legs on a daily basis.
What symptoms can varicose veins cause?
Apart from the purely cosmetic discomfort, varicose veins can cause more or less important and more or less associated symptoms:
- Leg heaviness
- Pain, discomfort, fatigue in the legs
- Swelling of the feet, ankles or calves
- Itching on the legs
- Impatience, restless legs
- Night cramps of the calves
- Skin eczema on the legs
Symptoms are generally worse at the end of the day (especially if you have been trampling), during the summer, after exposure to heat or after prolonged sitting (e.g. sitting travel).
On the other hand, they are improved by raising the legs, walking, physical exercise and cold (cold shower on the legs for example).
It should be noted that 20 to 25% of patients with varicose veins have no discomfort apart from the fact that the varicose veins are visible, even if they are very large. These are almost always people who have a high level of regular physical activity (walking, sports).
Can varicose veins cause serious complications?
In the vast majority of cases, varicose veins do not give rise to serious complications apart from discomfort, which can however be very painful.

photo 2
However, two main complications, of greater concern, can occur:
- Phlebitis: this is an acute complication that appears suddenly. . It is a varicose vein that becomes blocked with the formation of a clot (photo 2). The skin is red and usually painful. It requires the wearing of a compression stocking and an emergency anticoagulant treatment. This is the most frequent complication.
-

photo 3
The degradation of the skin until the appearance of a wound is a chronic complication that appears progressively in the lower part of the leg (photo 3). It’s called hypodermitis and varicose ulcer that are due to the permanent pressure of the varicose veins, which ends up damaging the skin, making it thick and fragile and leading to the emergence of the ulcer. It requires the wearing of compression stockings and long-term dressings and can take a long time to heal.
These complications are absolutely avoidable by treating the varicose veins early.
What can be done in the presence of varicose veins?
The first step is to consult a vascular specialist (vascular surgeon or vascular doctor, also called phlebologist or angiologist) to verify that the problem is indeed varicose veins and to assess it (by a clinical examination and a Duplex ultrasound scan) in order to propose a treatment.
Today, there are two main categories of medical and surgical treatments that are not very aggressive:
- Sclerotherapy (injection in the veins to “erase” them): concerns rather the very small veins (reticular varicose veins, telangiectasias, varicosities)
- Surgery : ASVAL method which preserves the saphenous vein (by microphlebectomy) and endovenous saphenous ablation (endovenous laser in particular) for more important varicose veins. Saphenous ablation is only indicated for the most degraded conditions. Saphenous ablation is only indicated for the most degraded conditions.
Wearing compression stockings is highly recommended to avoid complications, relieve symptoms (see above) and prevent worsening or relapse of varicose veins after they have been treated, but it can never eliminate varicose veins.
Taking products called venotonics, in the form of medication or dietary supplements, can be useful to relieve symptoms and prevent the degradation of veins, but as with compression stockings, it cannot be a solution to make varicose veins disappear.




